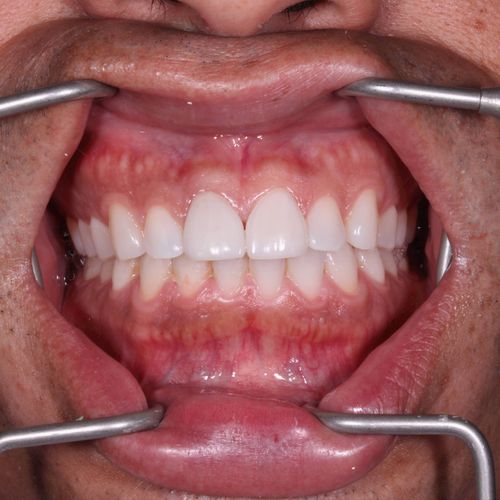












This case involved the complex reconstruction of fractured porcelain veneers on teeth #8 and #9, critical anterior teeth that play a pivotal role in both aesthetics and function. The case required not only restoring the structural integrity of the veneers but also ensuring that the final outcome would be indistinguishable from the surrounding natural dentition. Given the prominence of these teeth in the smile zone, the procedure demanded a meticulous approach to achieve optimal results.
The primary challenge was to achieve a seamless integration of shade, surface texture, micro-anatomy, and translucency map with the surrounding natural dentition. Specifically, the fractured veneers had to match the adjacent teeth in terms of hue, chroma, and value, while also replicating the intricate surface morphology and optical properties of natural enamel. Additionally, the patient presented with minor gingival recession at tooth #9, resulting in asymmetrical gingival architecture that further complicated the aesthetic considerations.
To address the gingival asymmetry, a laser gingivectomy was performed to re-contour the gingival architecture, creating a harmonious and balanced gum line that would complement the final veneer restorations. The choice of laser technology ensured precise tissue removal with minimal post-operative discomfort and expedited healing.
For the veneer reconstruction, Emax Class 2 porcelain veneers were selected due to their superior aesthetic properties and strength. A cut-back and opaquer technique was employed, allowing for the layering of porcelain to mimic the natural gradation of translucency seen in enamel. This approach also facilitated the creation of a lifelike opacity and fluorescence that blended seamlessly with the adjacent teeth. The careful selection of luting cement further ensured that the veneers maintained their intended shade and optical properties once bonded in place.
The final outcome showcased a significant improvement in both the aesthetics and functionality of the patient’s smile. The veneers not only restored the natural appearance of the teeth but also enhanced the overall symmetry and balance of the smile. The patient reported a marked increase in confidence, supported by positive feedback from peers. Comprehensive before-and-after documentation, including photographic evidence and patient testimonials, underscores the success of the procedure, demonstrating the critical importance of advanced restorative techniques in complex aesthetic cases.
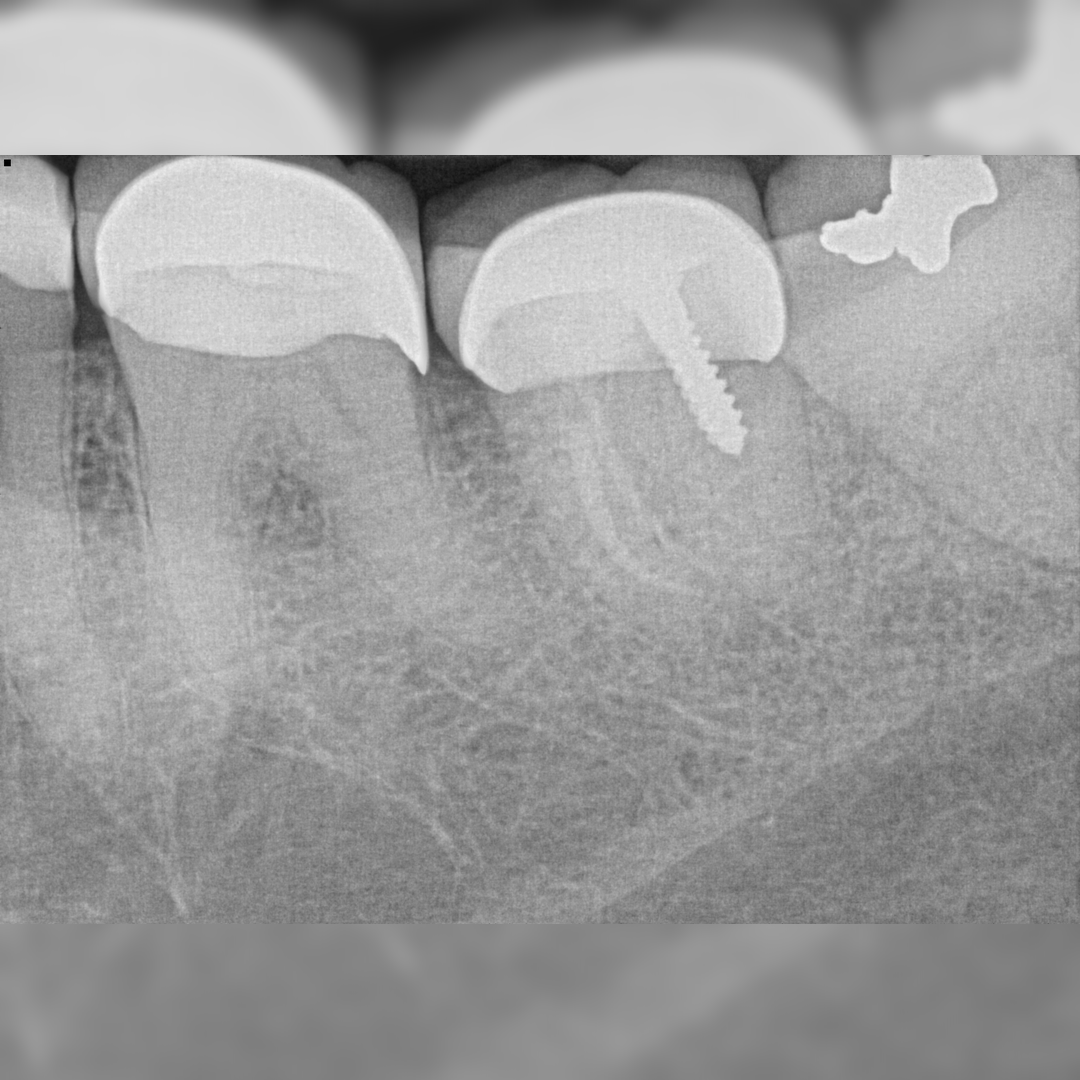
This case involved the endodontic management of a maxillary second molar, a tooth often associated with anatomical challenges and complexities due to its posterior location and root canal system variability. The treatment required precise diagnostic skills and advanced endodontic techniques to ensure the successful resolution of the pulp pathology while preserving the structural integrity of the tooth.
One of the primary challenges in this case was the accurate identification of the buccal roots on pre-operative periapical radiographs. The overlapping anatomical structures and potential curvature of the canals often obscure these details, making it difficult to visualize the complete root anatomy.
Additionally, the presence of an MB2 (mesiobuccal 2) canal, which is frequently missed due to its complex anatomy and location, further complicated the case. Limited access to the molar due to its posterior position and the patient’s restricted mouth opening posed additional difficulties, requiring meticulous technique to navigate the intricate root canal system effectively.
To address these challenges, a comprehensive pre-treatment evaluation was conducted, utilizing high-resolution digital radiography and, where necessary, cone-beam computed tomography (CBCT) to enhance the visualization of the root canal system. This diagnostic precision allowed for the identification of all canal orifices, including the elusive MB2 canal.
A collaborative treatment plan was developed in consultation with the patient, ensuring a clear understanding of the procedure’s complexity and the necessary steps to achieve a successful outcome.
Advanced endodontic techniques, including the use of magnification (dental operating microscope) and specialized nickel-titanium (NiTi) rotary instruments, were employed to navigate the limited access and intricate canal system. The use of a glide path and sequential shaping techniques ensured that all canals, including the MB2, were thoroughly debrided and shaped to facilitate effective obturation. Continuous irrigation with activated solutions was utilized to enhance disinfection, particularly in the apical third of the root canals.
The post-operative prognosis for this case remains highly favorable. A one-year follow-up examination, including clinical assessment and radiographic evaluation, revealed no signs of pain, swelling, or apical radiolucency, indicating successful resolution of the initial pathology and long-term preservation of the tooth. This outcome highlights the importance of thorough diagnostic procedures and the application of advanced endodontic techniques in managing complex molar cases.
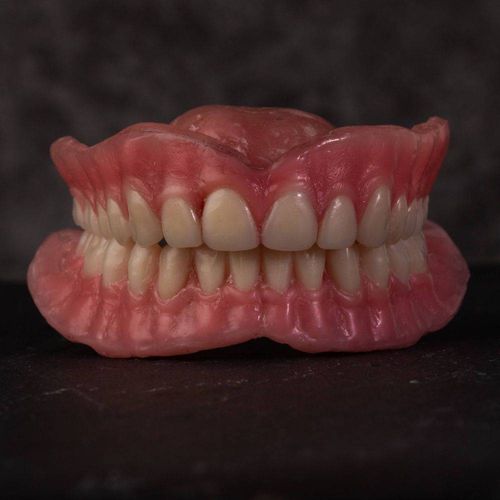
This case involved the comprehensive wax-up and fabrication of complete upper and lower dentures for a patient with a history of chronic edentulism. The procedure required a balance between aesthetics and functionality, with a particular focus on achieving a natural appearance and effective masticatory function. Given the complexities associated with long-term edentulism, the case demanded a careful and customized approach to ensure optimal results.
Patients with chronic edentulism often experience significant bone remodeling, leading to alveolar ridge resorption that complicates denture fabrication. In this case, the patient presented with pronounced bone loss, which posed a challenge in creating a denture that would provide both aesthetic appeal and functional stability.
A critical aspect of the treatment was ensuring proper gingival aesthetics, particularly in providing adequate lip support without compromising lip competence. This balance is crucial in preventing issues such as excessive vertical dimension of occlusion (VDO) or a collapsed appearance, both of which can affect the patient’s facial aesthetics and oral function.
Given the complexities of the case, it was essential to maintain direct oversight throughout the entire procedure, ensuring that every stage of the denture fabrication process aligned with the treatment objectives. This approach also minimized the risk of miscommunication with laboratory technicians, which could otherwise lead to suboptimal results.
The treatment began with a thorough examination, including an assessment of the need for pre-prosthetic surgery, such as alveoloplasty, to optimize the alveolar ridge for denture support. A detailed discussion with the patient helped manage expectations, aligning the final outcome with the patient’s aesthetic and functional desires.
Jaw relations were meticulously established using facebow transfer and were transferred to a fully adjustable articulator, allowing for precise replication of the patient’s mandibular movements. The wax-up try-in was a critical phase, focusing on both occlusion and aesthetics. Adjustments were made based on the patient’s feedback and clinical evaluation, ensuring that the final prosthesis would offer maximum comfort, function, and visual appeal.
The final outcome was highly satisfactory, with the dentures achieving optimal retention, occlusion, and aesthetics. The patient reported a significant improvement in both oral function and confidence. The prostheses provided excellent stability and comfort, while the gingival aesthetics and lip support restored a natural and youthful appearance. The successful management of this case underscores the importance of a comprehensive and patient-centered approach in the fabrication of complete dentures, particularly in cases complicated by significant bone resorption.
This case involved the restoration of a first maxillary premolar using a gold onlay, a choice made to strategically preserve the buccal cusp while ensuring long-term durability and function. The decision to use gold, known for its superior longevity and biocompatibility, was balanced with the need to maintain the tooth’s natural aesthetics, particularly in the smile zone.
One of the primary challenges in this case was addressing the patient’s concerns about the aesthetic impact of gold restorations, despite their well-documented advantages in terms of durability and biological compatibility.
The tooth presented with an existing restoration that extended deep into the gingival margin, complicating the preparation and requiring careful margin placement to ensure a seamless interface between the restoration and the tooth structure.
Additionally, the lingual cusp was significantly undermined due to previous restorative work, which increased the risk of fracture and necessitated a conservative yet effective approach to reinforce the tooth while minimizing further loss of healthy tooth structure.
Given the patient's preference for a durable solution that would not compromise aesthetics, a gold onlay was recommended as the most suitable treatment option. This decision followed a thorough discussion with the patient, outlining the benefits of gold in terms of strength, longevity, and its ability to preserve more of the natural tooth compared to full-coverage crowns.
The preparation design was meticulously planned to minimize the onlay’s visibility, particularly from the buccal aspect. Special attention was given to the marginal design, ensuring that the gold margins were kept narrow and placed subgingivally where possible to reduce their visibility. This approach preserved the buccal cusp and maximized the aesthetic outcome while still providing the necessary reinforcement to the compromised lingual cusp.
The onlay was fabricated using high-quality gold alloy, ensuring optimal fit and function. The use of a conservative preparation design not only preserved more of the natural tooth structure but also helped in maintaining the structural integrity and longevity of the restoration.
The patient expressed high satisfaction with the final outcome, particularly appreciating that the gold onlay remained discreet and did not compromise the appearance of her smile. The restoration provided exceptional durability and function while achieving an aesthetic result that met the patient’s expectations. The success of this case highlights the importance of combining conservative restorative techniques with patient-centered care, especially when addressing both functional and aesthetic concerns in dental restorations.
Anterior composite restoration on the maxillary lateral incisor.
Achieving an exact match in shade and surface texture for a small cavity located centrally on the labial surface of the maxillary lateral incisor.
A composite shade mock-up was meticulously performed prior to the procedure, ensuring a precise match and seamless integration with the surrounding tooth structure.
The outcome was highly successful, with the restoration blending perfectly, maintaining the natural aesthetics of the tooth.
This case involved the endodontic management of a simulated molar with severely curved mesial and distal roots, posing a significant challenge in achieving proper canal negotiation and cleaning. The case was part of an advanced endodontic training program, designed to test the clinician's ability to manage complex root canal anatomies.
The primary challenge was the severe curvature of both the distal and mesial roots, which significantly increased the risk of file separation, ledging, and transportation during canal instrumentation. Navigating these curvatures required precise control and technique to avoid compromising the integrity of the root canal system.
Additionally, the apical third of the canals was particularly difficult to access and shape due to the pronounced curvatures, necessitating a careful and methodical approach to ensure complete debridement without causing procedural errors.
A glide path was meticulously established to ensure safe and effective file progression through the curved canals. Maintaining patency throughout the procedure was critical, achieved through careful instrumentation and regular irrigation to prevent blockage and ensure smooth passage of files.
Manual preparation techniques were employed in the apical third, allowing for enhanced tactile feedback and control over the instrumentation process. This approach minimized the risk of canal transportation and ensured thorough cleaning and shaping, even in the most challenging areas of the canal system.
The use of flexible nickel-titanium (NiTi) files was also integral to navigating the severe curvatures, providing the necessary flexibility to conform to the root canal anatomy while maintaining cutting efficiency.
The case concluded with a highly positive outcome, with complete canal debridement and shaping achieved without any complications. The successful management of this complex endodontic anatomy highlights the importance of advanced techniques and precision in endodontic practice. The clinician's ability to adapt to challenging anatomical variations was critical in achieving the desired results, reinforcing the value of rigorous training and attention to detail in complex cases.
A 65-year-old female patient presented to the clinic seeking comprehensive dental treatment. Her primary concern was the replacement of her upper removable partial denture (RPD), which she found unretentive and unsatisfactory in both function and aesthetics. The patient expressed a desire for a solution that would improve her ability to chew and enhance the appearance of her smile, all within a limited budget.
This case presented several complex challenges that required careful consideration in developing a treatment plan:
Aesthetic Concerns:
The patient was unhappy with the aesthetics of her current dentition, particularly due to a severe midline shift and a large edentulous space where tooth #8 was missing. Additionally, the shade mismatch of an existing Emax crown on tooth #9 further compromised the overall appearance of her smile.
Occlusal Complications: The patient exhibited a deep bite, which complicated the occlusal scheme and required careful management to avoid exacerbating the condition during treatment.
Anatomical Challenges:
The presence of severely tilted lower third molars created difficulties in establishing a proper path of insertion for any prosthetic solution. This posed a significant challenge in ensuring that the final restoration would be both functional and comfortable for the patient.
Financial Constraints: The patient’s limited budget necessitated a phased approach to treatment, prioritizing critical needs while working within her financial limitations.
After a comprehensive examination, including detailed radiographs and a thorough discussion with the patient regarding her goals and constraints, a multi-phased treatment plan was developed to address both her functional and aesthetic concerns:
The final removable partial dentures provided the patient with superior retention, support, and stability, significantly enhancing her ability to chew and speak comfortably. Aesthetically, the dentures delivered a satisfactory result, addressing the midline shift and the large space for the missing tooth #8, while harmonizing with the surrounding dentition.
The patient was highly satisfied with the outcome, particularly appreciating the improved functionality and the overall appearance of her smile.
The midline shift was extreme , to the intended was not a complete correction but rather restoring it to only 4mm shift.
The phased treatment approach effectively balanced the patient’s functional needs, aesthetic desires, and budgetary constraints, demonstrating the importance of personalized treatment planning in achieving optimal patient outcomes.
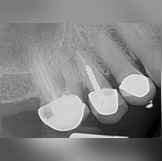
Dental implants have become increasingly popular among general practitioners (GPs), largely due to advancements in technology that have significantly improved osseointegration and long-term success rates. However, despite these technological improvements, implant failure rates have paradoxically risen over the past decade, often due to improper planning and execution during placement.
The primary challenge in this case involved achieving the correct bucco-lingual angulation during implant placement. Improper angulation can lead to an over-contoured lingual aspect of the crown, which necessitates the thinning of porcelain to correct occlusal discrepancies. This not only compromises the aesthetic outcome but also increases the risk of porcelain fracture and long-term implant failure. Additionally, ensuring proper implant placement in relation to the crestal bone level was critical to allow for an optimally functioning and aesthetically pleasing cement-retained crown.
To address these challenges, a buccal rotation of the implant was strategically planned and executed. This adjustment ensured that the final crown would have a more natural contour, reducing the need for excessive porcelain thinning. Moreover, the implant was positioned at an equi-crestal level to facilitate the use of a cement-retained crown, which provides better aesthetics and ease of maintenance compared to screw-retained crowns.
The treatment concluded with satisfactory results, both functionally and aesthetically. The patient benefited from a well-integrated implant with a crown that exhibited proper contour and occlusion, minimizing the risk of future complications. The strategic buccal rotation and careful positioning of the implant played a crucial role in the success of this case, demonstrating the importance of precise planning and execution in implant dentistry.
A 24-year-old female patient presented with aesthetic concerns, specifically expressing dissatisfaction with the shape of her maxillary lateral incisors. Her chief complaint was, "I don't like the shape of my laterals." The patient was highly motivated to improve the appearance of her smile but had budget constraints that limited her treatment options.
The primary challenge in this case was to deliver a solution that met the patient's aesthetic goals while remaining within her financial limitations. Porcelain veneers, known for their superior durability and aesthetic qualities, were the ideal treatment option; however, they were beyond the patient's budget.
Given the financial constraints, composite veneers were selected as an alternative. This option allowed for significant improvement in the shape and appearance of the lateral incisors at a lower cost. The composite veneers were carefully crafted and applied to enhance the symmetry and overall aesthetics of the patient's smile while preserving the natural tooth structure.
The patient was pleased with the immediate aesthetic improvement achieved with composite veneers. The treatment provided a cost-effective solution that met her aesthetic expectations. During the follow-up, the patient expressed interest in potentially upgrading to porcelain veneers in the future, recognizing their superior durability and long-term benefits, particularly when the composite material begins to show signs of wear or discoloration.
A 60-year-old male patient presented to the clinic with complete edentulism in both the upper and lower arches. The patient had been edentulous for several years, leading to significant bone resorption and facial changes associated with the loss of alveolar ridge height and support. His primary concern was the restoration of both aesthetics and function, as the lack of teeth had compromised his ability to chew and affected his facial profile.
The complete edentulism presented several challenges, particularly related to the extensive bone resorption, which affected the stability and retention of conventional dentures. The patient's facial musculature had adapted to the edentulous state, making it essential to carefully manage the vertical dimension of occlusion (VDO) to avoid over-closure or an unesthetic appearance.
Additionally, ensuring the proper fit and comfort of the dentures required careful consideration of the remaining alveolar ridge anatomy. Achieving a balance between aesthetics, functionality, and patient comfort was paramount, especially given the potential for decreased retention and stability in cases of severe ridge resorption.
After a comprehensive assessment, it was decided to fabricate complete upper and lower dentures. A meticulous treatment plan was devised, beginning with accurate impressions and bite registration to ensure the proper establishment of the occlusal plane and VDO. The use of custom trays and border molding techniques was employed to capture the full extent of the available ridge, enhancing the retention and stability of the final prostheses.
The dentures were fabricated with attention to detail in the arrangement of teeth, ensuring that they complemented the patient’s facial structure and restored a natural appearance. The choice of teeth and gingival contouring was made to provide a lifelike appearance, while also restoring the patient’s ability to chew effectively. Special attention was given to the fit of the dentures to avoid any discomfort or irritation, particularly in areas with thin mucosa overlying the resorbed ridges.
The patient was highly satisfied with the results, reporting a significant improvement in both his ability to eat and his overall appearance. The dentures provided excellent retention and stability, despite the challenges posed by the resorbed ridges. The successful restoration of the patient’s oral function and aesthetics greatly improved his quality of life, underscoring the importance of a tailored approach in the management of edentulous cases.
The psychological impact of tooth loss is often underestimated in clinical practice, yet it can significantly affect a patient's self-esteem and overall well-being. Immediate dentures offer a valuable solution, allowing patients to transition more comfortably by replacing teeth at the same visit as the extractions. This approach not only minimizes the emotional distress associated with edentulism but also provides immediate functional and aesthetic benefits. In some cases, patients prefer the immediate denture to closely mimic the position and shape of their existing anterior teeth, rather than opting for a sudden transformation to a 'perfect' smile.
The construction of immediate dentures presents several challenges. Accurately predicting the post-extraction ridge contour and ensuring that the denture fits properly without adjustments can be difficult. Moreover, aligning patient expectations with clinical outcomes, especially when aiming to replicate the natural irregularities of their existing teeth, requires a careful balance of technical precision and aesthetic judgment. Ensuring that the denture provides sufficient retention and stability immediately after surgery is another key concern, given the changes in the oral environment that occur post-extraction.
Addressing these challenges involves meticulous planning and communication with the patient. A thorough pre-extraction assessment, including diagnostic impressions and bite registration, is essential for crafting a denture that fits well and meets aesthetic expectations. In some cases, a staged approach may be recommended, where minor adjustments are made after initial healing to optimize fit and comfort. Patient education is also critical, ensuring they understand the temporary nature of immediate dentures and the potential need for relining or replacement as the healing process progresses.
The successful delivery of immediate dentures can significantly enhance patient satisfaction, offering an immediate solution that addresses both functional and aesthetic concerns. Patients often express relief at not having to experience a period of edentulism, and the psychological benefits are notable. Follow-up care is crucial to monitor the fit of the dentures and make necessary adjustments, ensuring long-term comfort and functionality. This approach not only helps in maintaining oral health but also supports the patient's emotional well-being during what can be a challenging transitional period.
Survey crowns are a specialized restorative option that I was first introduced to during my training at UCLA. These crowns play a crucial role in optimizing abutment contours to achieve a more favorable design for Removable Partial Dentures (RPDs). They are particularly indicated for teeth with extensive restorations, endodontically treated teeth, or those with contours that cannot be adequately managed with enameloplasty. The process involves fabricating a wax-up of the survey crown, followed by re-surveying the cast to ensure that the contours of the wax-up align precisely with the predetermined design parameters for the RPD framework. This technique ensures that the final restoration supports the mechanical and aesthetic demands of the prosthesis.
The primary challenge with survey crowns lies in achieving the precise modification of abutment contours required for optimal RPD design. This necessitates a deep understanding of both prosthodontic principles and the specific mechanical needs of the RPD framework. Additionally, balancing the functional requirements of the crown with the aesthetic considerations can be difficult, especially in cases where the abutment teeth are in the esthetic zone. The risk of over-reduction or under-preparation of the tooth structure also presents a significant challenge, as it could compromise the structural integrity or the retentive capacity of the crown.
To address these challenges, a meticulous approach was adopted, beginning with a thorough diagnostic work-up that included radiographic analysis and detailed planning of the RPD design. The wax-up was carefully fabricated to meet the specific contour requirements, ensuring that it provided the necessary undercuts and guiding planes while preserving the esthetics and function of the abutment teeth. The cast was then re-surveyed to confirm that the final contours met the predetermined design criteria. This process was supported by close collaboration with the dental laboratory, ensuring that every step was executed with precision.
The final outcome was highly successful, with the survey crowns providing the necessary structural support and contour modification for the RPD. The crowns not only enhanced the retention and stability of the prosthesis but also met the aesthetic expectations of the patient. This case underscores the importance of integrating advanced restorative techniques with comprehensive prosthodontic planning to achieve optimal results in complex rehabilitative cases.
"It feels like natural teeth again" were the first words my patient uttered after receiving his implant-supported crowns. The patient had been using a removable partial denture (RPD) to replace his posterior teeth for the past five years. While implants have become increasingly popular among general practitioners, advancements in technology have significantly improved their osseointegration properties. However, implant failure rates have been rising over the past decade. Proper treatment planning and thorough preoperative workup are critical in enhancing the success rate and longevity of implants.
The primary challenge in this case was restoring all the posterior molars. On the right side, the patient had only the maxillary first molar remaining, so we focused on restoring just that molar with an implant-supported crown. This selective restoration required careful consideration of occlusal balance and functional load distribution to ensure long-term success and patient satisfaction.
To address the challenges, we conducted a comprehensive treatment plan that included detailed diagnostic imaging and occlusal analysis. The implant placement was meticulously planned to ensure optimal positioning, angulation, and depth, taking into account the limited space and existing occlusal scheme. A custom abutment was used to provide the best possible fit and aesthetics for the crown, ensuring that it integrated seamlessly with the patient’s natural dentition.
The patient was highly satisfied with the outcome, particularly noting the natural feel and comfort of the implant-supported crown. The restoration not only improved his chewing efficiency but also enhanced his overall oral health by eliminating the need for an RPD on the right side. This case highlights the importance of precise treatment planning and execution in achieving successful implant restorations.
This case involves a retreatment of the maxillary first molar, where the patient presented with persistent discomfort and signs of infection despite previous endodontic treatment. The initial radiograph revealed a complex canal anatomy with residual infection that required meticulous retreatment.
The primary challenges in this case included navigating the complex canal system and removing the previous obturation material. Additionally, a post was present in the adjacent premolar, complicating the access and necessitating careful instrumentation to avoid iatrogenic damage. Another significant challenge was the management of apical infection and ensuring complete disinfection of the canal space.
Advanced imaging techniques, such as CBCT, were utilized to better understand the canal morphology and guide the retreatment process. The existing gutta-percha was removed using rotary instruments, and the canals were re-instrumented and thoroughly irrigated using an enhanced protocol with sodium hypochlorite and EDTA. The use of a bioceramic sealer helped to ensure a hermetic seal, addressing both the complexity of the anatomy and the persistent infection.
Post-operative radiographs confirmed the successful obturation of all canal spaces, with the infection being resolved. The patient reported significant improvement in symptoms, and the prognosis for the tooth is favorable. The treatment of the adjacent premolar, where a post was present, was addressed in a subsequent appointment to ensure long-term stability and function.
1. Siqueira JF, Rocas IN. Microbiology and Treatment of Endodontic Infections. In: Ingle JI, Bakland LK, Baumgartner JC, editors. Ingle’s Endodontics. 6th ed. Hamilton: BC Decker Inc; 2008. p. 1019–54.
2. Torabinejad M, Walton RE. Endodontics: Principles and Practice. 5th ed. St. Louis: Elsevier; 2014.
A 45-year-old patient presented with persistent discomfort in the lower left molar region, despite undergoing previous root canal treatment. Clinical examination revealed tenderness on percussion and slight swelling, indicative of a residual infection. The adjacent premolar had a post, complicating access to the affected molar. Radiographic analysis, including a CBCT scan, confirmed the presence of a periapical lesion in the treated molar, necessitating retreatment.
The retreatment of the molar presented several challenges, including:
To address these challenges, the following advanced techniques were employed:
The retreatment was successful, with the patient reporting significant relief from discomfort. Post-operative radiographs showed complete resolution of the periapical lesion, and the tooth was restored with a new crown. The patient was followed up at 3, 6, and 12 months, with continued positive outcomes. The prognosis for the treated molar is excellent, with no signs of recurrent infection.
This case study involves a patient presenting with advanced Mesio-Occlussal cavity on the maxillary second molar. The objective was to eliminate pain and restore the tooth's functionality .
The primary challenges included addressing the complex anatomy of the maxillary second molar and accessability due to limited mouth opening.
The treatment strategy involved careful negotiation the MB canal curvature, followed by thorough cleaning and shaping of the canal system using advanced endodontic instruments and irrigation protocols. The canals were then obturated with bioceramic sealers to achieve a hermetic seal, followed by a composite core buildup to restore the structural integrity of the tooth.
Postoperative radiographs (as shown) revealed excellent obturation with complete resolution of the periapical pathology. The patient reported immediate relief of symptoms and has been asymptomatic during follow-up appointments. This case highlights the importance of precision in treatment procedures, utilizing advanced materials and techniques to achieve successful outcomes even in challenging cases.
A patient presented to our clinic with significant discomfort in the upper right quadrant, shortly after the placement of a new crown. Despite the meticulous execution of the crown procedure, the patient continued to experience pain, prompting further investigation.
Upon conducting a thorough clinical and radiographic examination, we identified a periapical radiolucent lesion beneath the recently placed crown, which otherwise demonstrated perfect sealing. This posed a unique challenge: the patient was reluctant to undergo the replacement of the crown, which limited our treatment options.
To address the underlying issue while preserving the crown, we implemented the following solutions:
Post-operative radiographs, as illustrated, showcased excellent obturation with no residual signs of the lesion. The patient experienced immediate relief from the initial symptoms and has remained asymptomatic during all subsequent follow-up appointments. This case underscores the significance of innovative and conservative approaches in preserving dental restorations while effectively managing complications.
Removable Partial Denture (RPD) design is a critical aspect of restorative dentistry, involving various components that work together to restore function, aesthetics, and comfort for patients with partial edentulism. These components include major connectors, minor connectors, direct retainers, indirect retainers, and rests. Each element serves a specific purpose, ensuring the stability and retention of the prosthesis, while also distributing functional forces appropriately. The design of an RPD must be meticulously tailored to the individual patient's oral condition, requiring careful consideration of factors such as the number of remaining teeth, the condition of the supporting structures, and the patient's overall oral health.
One of the primary challenges in RPD design is the temptation to delegate this task entirely to a lab technician. While lab technicians are skilled in fabricating prostheses, the clinical perspective of a dentist is crucial in the design process. The dentist's understanding of the patient's oral anatomy, functional dynamics, and specific clinical needs allows for a more personalized and effective design. Additionally, each RPD case presents unique challenges; therefore, the design process is far from a one-size-fits-all approach. A standardized design could lead to poor fit, discomfort, and even damage to the remaining teeth or soft tissues.
The most effective approach to RPD design involves close collaboration between the dentist and the lab technician, with the dentist taking the lead in the initial design phase. This ensures that the RPD is customized to meet the patient's specific needs, with the dentist making informed decisions about the selection and placement of components. For example, the dentist can determine the most appropriate major connector based on the arch form and tissue conditions, select direct retainers that offer optimal retention without compromising tooth structure, and position rests to provide adequate support and prevent unwanted movement of the prosthesis. This collaborative approach not only improves the fit and function of the RPD but also enhances patient satisfaction and long-term oral health.
By prioritizing the dentist's role in RPD design, the final prosthesis is more likely to achieve its intended goals of restoring function, aesthetics, and comfort. Patients benefit from a prosthesis that is tailored to their unique oral condition, leading to improved retention, stability, and overall satisfaction. Moreover, the dentist's involvement in the design process reduces the risk of complications, such as tissue irritation or tooth damage, thereby contributing to better long-term outcomes. Ultimately, the success of an RPD hinges on the meticulous design process, which should be spearheaded by the dentist rather than delegated entirely to the lab technician
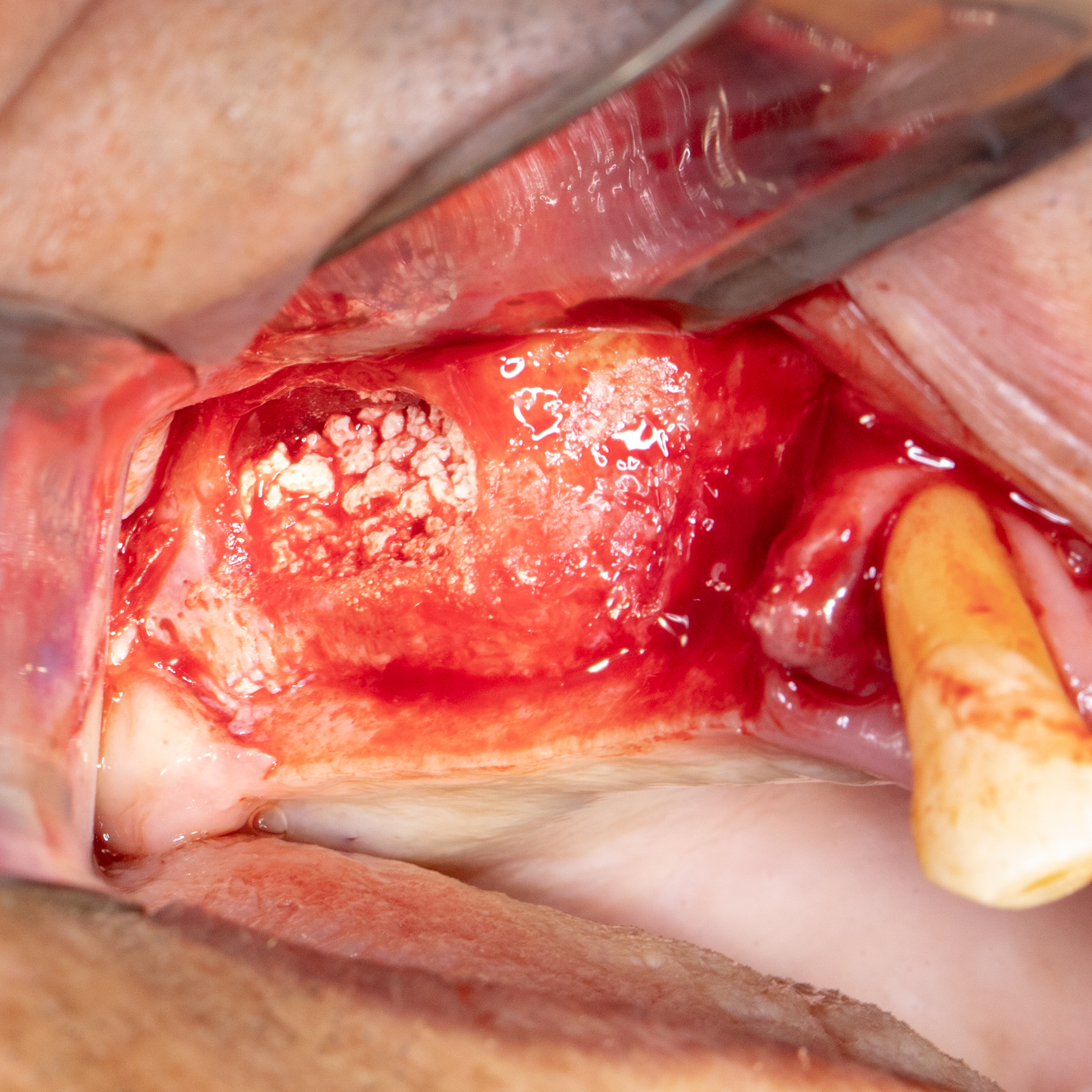
Open sinus lift procedures have become an indispensable technique in implant dentistry, especially when faced with insufficient vertical bone height in the posterior maxilla. This case involved a patient requiring dental implants in the upper molar region, where the maxillary sinus presented a significant challenge due to its proximity. The procedure was carefully planned using advanced imaging techniques to ensure precise and predictable outcomes.
The primary challenge was the reduced bone height in the posterior maxilla, with less than 3 mm of bone available for implant placement. Ensuring the integrity of the Schneiderian membrane during the procedure was also paramount, as any perforation could lead to complications such as sinusitis or graft failure.
A lateral window approach was selected for this open sinus lift procedure, allowing for direct visualization and careful elevation of the Schneiderian membrane. To enhance the bone regeneration process, a combination of autogenous bone and a xenograft material was used, promoting both osteoconduction and osteoinduction. Meticulous technique and the use of piezoelectric surgical tools were employed to minimize trauma and ensure the precise elevation of the sinus membrane. Antibiotic prophylaxis and postoperative care were carefully managed to reduce the risk of infection and ensure optimal healing.
The procedure was successful, with no complications reported during or after surgery. The bone graft integrated well with the native bone, providing a stable foundation for future implant placement. Follow-up radiographs showed significant bone gain in the maxillary sinus area, and the patient reported minimal discomfort postoperatively. This case highlights the effectiveness of an open sinus lift in managing complex cases with severe bone loss, paving the way for successful implant placement and long-term dental restoration.
